Ulcerative Colitis
Back when I first began blogging, I wrote a post with a basic overview of ulcerative colitis (UC). Back then, I’d only had the disease for three years and I still didn’t have a full grasp on what UC really was. That was nearly ten years ago now and I’ve been living with UC for nearly 14 years.
Since I began blogging, I’ve really delved into what UC is. I’ve conducted hours of research, chatted with doctors, watched videos and really learned, in great detail, what ulcerative colitis is and how it affects the body. With all that being said, I want to encourage everyone to PLEASE read my disclaimer and remember that I am not a doctor or medical professional.
So what is it?
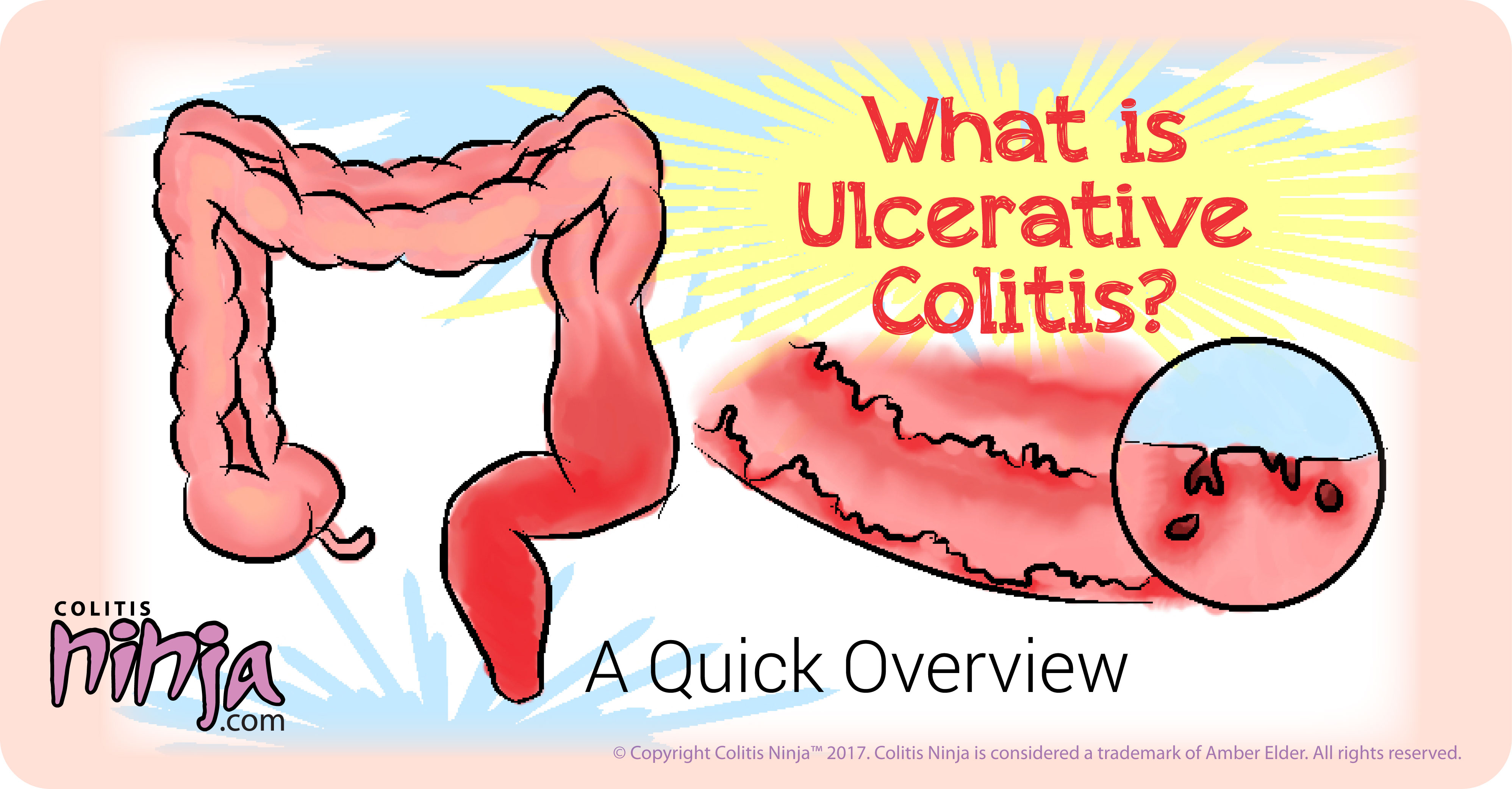
Basically, ulcerative colitis, or UC, is one of two main types of inflammatory bowel disease (IBD). Patients may experience many extra-intestinal manifestations, but the main symptoms of the disease reside in the colon and rectum. UC, like Crohn’s, is considered to be an autoimmune disease. In general, UC begins in the rectum and, as the disease progresses, works its way upward.
Symptoms may include the following:
- rectal bleeding
- frequency/urgency in bowel movements
- bloody diarrhea
- pus or mucus in stool
- fever
- rapid weight loss
- anemia
- pain/cramping
- nausea/vomiting
Types of UC
There are five main types of UC, including, ulcerative proctitis, proctosigmoiditis, left-sided colitis, pancolitis and fulminant colitis. Each one depends on the severity of the disease. I will go over these in detail.
1) Ulcerative Proctitis
Ulcerative proctitis is limited to rectum involvement. This is the mildest form of UC and the only symptom may be bleeding.
2) Proctosigmoiditis
This is also a milder form of the disease and is also known as distal colitis. It, too, involves the rectum, but also includes inflammation in the lower sigmoid colon (for more detail on the anatomy of the colon, click here). Symptoms may include bloody diarrhea, cramping, pain and tenesmus.
3) Left-Sided Colitis
Left-sided colitis is considered to be a moderate form of the disease which also includes rectum involvement and up through the sigmoid colon to the transverse colon. Bloody diarrhea, cramping, pain on the left side and weight loss may be present.
4) Pancolitis
Pancolitis, also known as extensive colitis, is a moderate to severe form of the disease. A colonoscopy will reveal the severity. Pancolitis stretches the entire length of the colon. Symptoms include bloody diarrhea, severe pain and cramping, anemia, weight loss, nausea and vomiting. Some patients also have what is called backwash ileitis. This is when the terminal ileum also becomes inflamed and could involve some erosion of the ileocecal valve.
5) Acute Severe Ulcerative Colitis
Also known as fulminant colitis, acute severe ulcerative colitis is the rarest form of the disease. It is also the most damaging and dangerous. Patients with fulminant colitis are at a higher risk for bowel perforations and toxic megacolon; both of which can be deadly.
Characteristics of UC
Pseudo Polyps
Ulcerative colitis exhibits pseudo polyps. These polyps are not actually polyps at all, but the surviving mucosa of the colon that has not been eroded away by inflammation and ulceration.
Wall Depletion
As mentioned, the lining of the colon thins and erodes away which is why patients with UC are at risk for bowel perforations. This is called wall depletion.
Loss of Haustra
The haustra gives the colon a segmented appearance. These pouches help move waste/feces along through the colon. Extensive inflammation causes the haustra to be destroyed, contributing to diarrhea and frequency of bowel movements.
Treatment for Ulcerative Colitis
The treatments used for UC are as follows:
- Aminosalicylates (such as Colazal, Lialda and Rowasa)
- Corticosteroids (i.e. Prednisone)
- Azathioprine (Imuran)
- Cyclosporine
- Biologics (Remicade, Simponi, Cimzia, etc.)
- Antibiotics
- Surgery
While there are some out there who consider surgery to be curative for UC, many others do not. There are many reasons for this. The main reason being the fact that UC is an autoimmune disease and therefore you cannot simply remove the disease by removing the organ that is affected. You can read my post on the subject here, and you can also read this post by my friend Rasheed Clarke, as well as this post by my friend Amber Tresca.
So, there you have it. I hope this helped you understand better what UC is. Again, please remember that I am not a healthcare professional and therefore cannot help you diagnose or treat any diseases. Please see my disclaimer.



